A clinical documentation cheat sheet PDF serves as a concise guide for healthcare professionals, streamlining patient assessments, treatment plans, and legal compliance, ensuring accurate and efficient documentation practices.
1.1 What is a Clinical Documentation Cheat Sheet?
A clinical documentation cheat sheet is a concise, user-friendly guide designed to assist healthcare professionals in accurately and efficiently documenting patient encounters. It typically includes key elements such as patient identification, medical history, assessment findings, diagnoses, treatment plans, and legal considerations. These tools are often presented in PDF format for easy access and reference. They serve as quick reminders of essential documentation standards, ensuring compliance with regulatory requirements and promoting consistent, high-quality care. Cheat sheets may also include templates, checklists, or examples to streamline the documentation process. By providing a structured framework, they help reduce errors and improve the clarity of medical records, ultimately supporting better patient outcomes and seamless communication among healthcare teams.
1.2 Importance of Clinical Documentation in Healthcare
Accurate and comprehensive clinical documentation is the foundation of high-quality patient care, serving as a legal and professional record of all healthcare encounters. It ensures continuity of care, facilitates effective communication among healthcare providers, and supports patient safety by providing a clear understanding of diagnoses, treatments, and outcomes. Proper documentation also protects healthcare professionals and organizations legally, serving as evidence of adherence to standards of care. Additionally, it plays a critical role in billing, insurance reimbursement, and compliance with regulatory requirements. By maintaining detailed and precise records, healthcare providers can enhance patient trust, improve treatment decisions, and ensure transparency in care delivery. Ultimately, robust clinical documentation is essential for delivering efficient, coordinated, and patient-centered healthcare services.

Key Components of a Clinical Documentation Cheat Sheet
A clinical documentation cheat sheet typically includes patient identification, medical history, assessment, diagnosis, treatment plans, and legal considerations, ensuring comprehensive and accurate healthcare documentation practices.
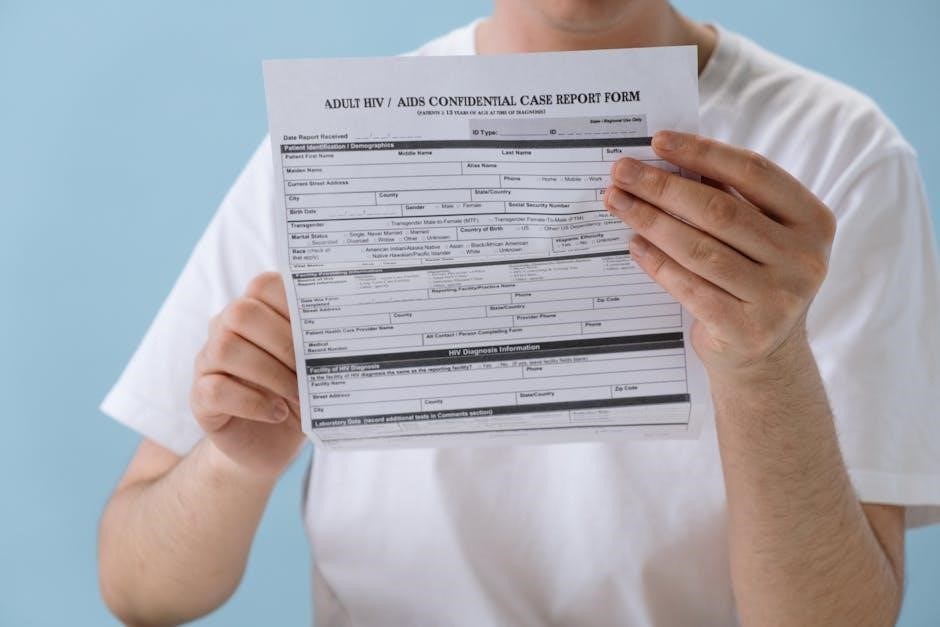
2.1 Patient Identification and Basic Information

Patient identification and basic information are foundational elements in clinical documentation. This section typically includes the patient’s name, date of birth, medical record number, and contact details. Accurate identification ensures patient safety and proper record-keeping. Basic information may also cover emergency contacts, insurance details, and language preferences. This data is essential for care coordination and legal compliance. Ensuring clarity and accuracy in this section helps prevent mix-ups and errors in treatment plans. Proper documentation of patient identification is critical for maintaining confidentiality and adherence to healthcare regulations. This section serves as the cornerstone for all subsequent documentation, making it vital for healthcare professionals to prioritize its accuracy and completeness.
2.2 Medical History and Patient Profile
The medical history and patient profile section captures essential details about the patient’s health background. This includes chronic conditions, past surgeries, allergies, medications, and family health history. Documenting lifestyle factors such as smoking, alcohol use, and occupation provides context for treatment. The patient profile may also include demographic information, behavioral or cognitive status, and communication preferences. Accurate and detailed documentation of this information aids in diagnosis, treatment planning, and continuity of care. It also helps identify potential risks and ensures personalized care. Clinicians rely on this data to make informed decisions, making it a critical component of effective clinical documentation. Ensuring completeness and accuracy in this section is vital for patient safety and optimal outcomes.
2.3 Assessment and Diagnosis
The assessment and diagnosis section outlines the clinician’s evaluation of the patient’s condition. It includes clinical judgment, physical examination findings, and diagnostic test results. This section summarizes the patient’s diagnoses, differentials, and the rationale behind them. Clear documentation of the assessment and diagnosis is crucial for guiding treatment decisions and ensuring continuity of care. It also supports accurate coding and billing processes. Examples of diagnoses may include acute or chronic conditions, such as acute osteomyelitis or chronic osteomyelitis, with notes on severity and progression. Proper documentation ensures that all healthcare team members are aligned on the patient’s care plan and outcomes. This section is a cornerstone of effective clinical documentation, enabling precise and targeted patient management.
2.4 Treatment Plan and Progress Notes
The treatment plan outlines the course of action for managing the patient’s condition, including medications, therapies, and follow-up appointments. Progress notes track the patient’s response to treatment, documenting improvements, setbacks, or adjustments to the care plan. This section ensures continuity of care and communication among healthcare providers. It also serves as a legal record of the patient’s journey and treatment outcomes. Accurate documentation in this section is vital for justifying medical necessity and skilled care, particularly for coding and billing purposes. Regular updates in progress notes reflect the patient’s evolving needs and the effectiveness of interventions. This section is essential for maintaining clear, actionable, and patient-centered documentation. It supports seamless coordination of care and ensures all team members are informed.
2.5 Legal and Compliance Considerations
Accurate and complete clinical documentation is essential for legal protection and compliance with healthcare regulations. Proper documentation ensures adherence to standards like HIPAA, protecting patient confidentiality and avoiding legal disputes. It also supports coding accuracy, preventing fraud and abuse. Documentation must be timely, legible, and signed by authorized personnel to maintain its validity. Incomplete or altered records can lead to legal consequences and reimbursement issues. Regular audits and reviews of documentation ensure compliance with regulatory requirements. Staying informed about updates in laws and guidelines is critical to maintaining proper documentation practices. This section emphasizes the importance of ethical and lawful documentation to safeguard both patients and healthcare providers. Proper legal compliance ensures trust and integrity in patient care delivery.

Best Practices for Effective Clinical Documentation
Ensure clarity, accuracy, and timeliness in documentation. Use templates for consistency and efficiency. Regularly review and update records to reflect patient progress and regulatory changes.
3.1 Tips for Accurate and Comprehensive Documentation
Accurate documentation starts with clear and concise language, avoiding abbreviations. Include patient identifiers, dates, and times. Document chief complaints, histories, assessments, and plans thoroughly. Use standardized templates to ensure consistency. Double-check for errors and omissions. Stay updated with medical terminology and coding guidelines. Prioritize patient-specific details to support medical necessity. Regularly review and update records to reflect current patient status. Ensure compliance with legal and regulatory standards. Leveraging technology, such as voice-to-text or AI tools, can enhance efficiency without sacrificing detail. Finally, always maintain patient confidentiality and adhere to HIPAA guidelines in all documentation practices.
3.2 Avoiding Common Documentation Errors
To maintain high-quality documentation, avoid common errors such as illegible handwriting, incomplete information, or vague terminology. Ensure all entries are dated, timed, and signed. Never leave blank spaces or use excessive abbreviations. Avoid altering or deleting entries, as this can lead to legal issues. Always document objective findings, patient responses, and care plans clearly. Use standardized terminology and avoid subjective interpretations. Regularly review documentation for accuracy and completeness. Address discrepancies promptly and maintain patient confidentiality. Implementing electronic health records (EHRs) can reduce errors and improve clarity. Finally, stay informed about documentation standards and best practices to minimize risks and ensure compliance with regulatory requirements.
3.3 Staying Updated with Regulatory Changes
Remaining informed about regulatory updates is crucial for accurate and compliant documentation. Stay abreast of changes in coding guidelines, such as ICD-10 and CPT updates, to ensure documentation aligns with billing requirements. Familiarize yourself with federal and state laws, including HIPAA, to maintain patient confidentiality and avoid legal risks. Regularly review updates from CMS and other regulatory bodies to understand new documentation standards. Participate in training sessions and workshops to stay current on best practices. Subscribe to professional newsletters and follow industry leaders for timely updates. Understand how documentation impacts reimbursement and quality metrics. Use cheat sheets and guides to quickly reference new requirements. Documenting accurately ensures compliance and supports patient care continuity.
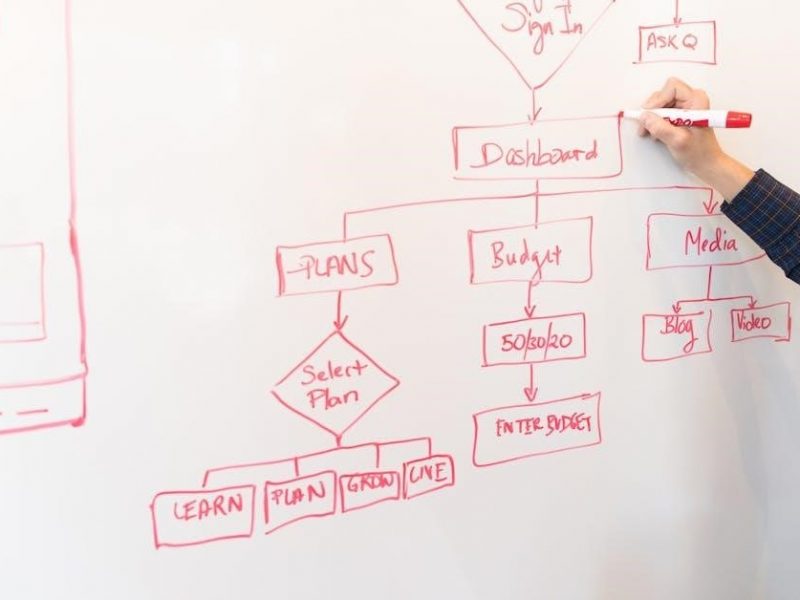
3.4 Using Templates for Efficiency
Using templates is a powerful way to enhance efficiency in clinical documentation. Pre-designed templates streamline the documentation process by providing structured formats for common patient encounters, reducing the time spent on paperwork. Standardized templates ensure consistency in documentation, making it easier for healthcare teams to review and understand patient information. Templates can be tailored to specific needs, such as nursing assessments or progress notes, ensuring that critical details are not overlooked. Downloadable PDF templates are widely available, offering ready-to-use solutions for various clinical scenarios. By leveraging templates, healthcare professionals can focus more on patient care and less on documentation, improving overall workflow and accuracy. This approach also helps maintain compliance with regulatory requirements, ensuring that documentation meets legal and billing standards.

Examples of Clinical Documentation Cheat Sheets
Clinical documentation cheat sheets include Nursing Head-to-Toe Assessment, Mental Health Progress Notes, Medical Necessity examples, and Acuity of Conditions, providing structured guides for accurate and efficient documentation practices.
4.1 Nursing Head-to-Toe Assessment Cheat Sheet
A Nursing Head-to-Toe Assessment Cheat Sheet offers a structured checklist for evaluating patients, starting with vital signs and progressing through body systems. It ensures comprehensive documentation, from cardiovascular to neurological assessments, aiding nurses in organizing findings efficiently. This tool is especially useful for new graduates, providing clear prompts to avoid missing critical details. By following the cheat sheet, nurses can systematically document observations, ensuring thorough and accurate patient records. This resource is often downloadable as a PDF, making it easily accessible for quick reference during assessments. Its simplicity and clarity make it an indispensable aid in daily clinical practice, enhancing both patient care and documentation quality.
4.2 Mental Health Progress Notes Cheat Sheet
The Mental Health Progress Notes Cheat Sheet is a concise, downloadable PDF designed for professionals in mental health. It provides a structured format for documenting patient progress, including mood, cognition, and behavioral observations. The cheat sheet ensures consistency and completeness in notes, aiding in tracking treatment efficacy and patient responses. It typically includes sections for diagnosis, interventions, and plans, making it a valuable tool for therapists and clinicians. By standardizing documentation, it enhances communication among healthcare teams and supports accurate billing and legal compliance. This resource is particularly beneficial for maintaining organized and precise records, ultimately improving patient care outcomes in mental health settings.

4.3 Medical Necessity and Skilled Care Examples
The Medical Necessity and Skilled Care Examples section provides practical illustrations of documentation for treatments requiring specialized skills. It includes examples like acute osteomyelitis, chronic osteomyelitis, and acute peritonitis, highlighting the need for skilled intervention. These examples demonstrate how to document complex conditions, ensuring clarity on why specific treatments are medically necessary. The section emphasizes the importance of detailing patient comorbidities, disease progression, and the rationale for skilled care. By providing clear, evidence-based examples, this resource helps healthcare professionals justify medical necessity effectively, ensuring compliance with regulatory standards and accurate reimbursement. These examples are essential for maintaining precise and defensible documentation in clinical settings.
4.4 Acuity of Conditions Documentation
Acuity of conditions documentation focuses on categorizing patient diagnoses as acute, chronic, or acute on chronic. This classification helps guide treatment intensity and resource allocation. For example, acute osteomyelitis requires immediate intervention, while chronic osteomyelitis involves long-term management. Similarly, acute peritonitis demands urgent care, unlike its chronic counterpart. Documenting acuity ensures clear communication among healthcare providers, aligns treatment plans with patient needs, and supports compliance with clinical guidelines. Accurate acuity documentation also aids in justifying medical necessity and skilled care, ensuring precise billing and legal protection. By clearly defining acuity levels, healthcare professionals can deliver targeted, effective care while maintaining thorough and defensible records. This section provides examples to help clinicians document acuity effectively, enhancing patient outcomes and operational efficiency. Proper acuity documentation is vital for seamless care coordination and optimal resource utilization.

Tools and Resources for Clinical Documentation
Various tools and resources, such as downloadable templates, CDI guides, specialized software, and training materials, are available to enhance efficiency and accuracy in clinical documentation practices.

5.1 Downloadable PDF Templates and Guides
Downloadable PDF templates and guides provide structured frameworks for clinical documentation, ensuring consistency and completeness. These resources often include pre-designed forms for patient assessments, progress notes, and treatment plans. For example, nursing head-to-toe assessment templates offer detailed checklists for evaluating patients systematically. Mental health progress notes templates guide professionals in documenting client progress and treatment responses. Additionally, guides for medical necessity and skilled care documentation help clinicians justify treatment plans with clear evidence. Many templates are customizable, allowing healthcare providers to tailor them to specific patient needs or practice settings. These tools not only save time but also reduce errors, ensuring that documentation meets regulatory standards. By leveraging these resources, healthcare professionals can enhance the quality and efficiency of their documentation practices. These templates are widely available online, making them accessible to a broad range of users.
5.2 Clinical Documentation Improvement (CDI) Resources
Clinical Documentation Improvement (CDI) resources are essential tools for enhancing the accuracy, completeness, and compliance of healthcare documentation. These resources include guidelines, training materials, and best-practice frameworks designed to help healthcare professionals improve documentation quality. CDI resources often focus on specific areas, such as coding accuracy, medical necessity documentation, and compliance with regulatory requirements. They may also provide tips for avoiding common documentation errors and strategies for staying updated on changing regulations. By leveraging CDI resources, healthcare providers can ensure their documentation is precise, defensible, and aligned with industry standards. These tools are particularly valuable for clinicians, coders, and documentation specialists seeking to optimize patient care and operational efficiency. Regular updates and access to expert insights make CDI resources indispensable for continuous improvement in clinical documentation practices.
5.3 Software and Apps for Streamlined Documentation
Software and apps designed for clinical documentation offer healthcare professionals efficient tools to streamline the documentation process. These solutions often include features like voice recognition, pre-built templates, and real-time data access, reducing the time spent on manual entry. Apps such as Mentalyc’s Progress Notes Cheat Sheet provide structured formats for mental health professionals, ensuring consistency and accuracy. Additionally, some platforms integrate with electronic health records (EHRs), allowing seamless data sharing and retrieval. These tools also offer customization options, enabling users to tailor documentation to specific patient needs or organizational requirements. By leveraging advanced software, healthcare providers can enhance productivity, reduce documentation errors, and improve compliance with regulatory standards, ultimately delivering better patient care.
5.4 Training and Educational Materials
Training and educational materials are essential for mastering clinical documentation. These resources include guides, webinars, and workshops that cover best practices, regulatory updates, and practical tips. For instance, the Basel Institute for Clinical Epidemiology offers tutorials on data documentation, while Nursing Head-to-Toe Assessment Cheat Sheets provide structured checklists for nurses. Additionally, courses from institutions like Trans-Baikal State University focus on improving clinical documentation skills. These materials emphasize accuracy, completeness, and compliance, ensuring healthcare professionals can document effectively. They also address common pitfalls and provide examples of well-structured documentation. By leveraging these educational tools, healthcare providers can enhance their proficiency, reduce errors, and deliver high-quality patient care while maintaining regulatory adherence. Such resources are invaluable for both new and experienced professionals.
A clinical documentation cheat sheet PDF is an indispensable resource for healthcare professionals, offering a structured approach to accurate and efficient documentation. By providing essential guidelines, checklists, and examples, it ensures compliance with legal and regulatory standards while improving patient care outcomes. These tools are adaptable to various healthcare settings and specialties, making them a versatile asset for clinicians. Regular updates and training materials further enhance their utility, helping professionals stay informed about best practices and regulatory changes. Ultimately, a well-crafted clinical documentation cheat sheet not only streamlines workflows but also supports continuous improvement in healthcare delivery. It is a valuable companion for both seasoned professionals and those new to the field, fostering excellence in documentation and patient care.